You are at a cardiac arrest on the ward. The nurse informs you the patient rapidly deteriorated when their fluids were disconnected from their central line. That is when you notice the central line lumens have been left open to air. You are suspicious of an air embolus, which is confirmed on admission to ICU, and despite resuscitative attempts the patient dies two days later. The unfortunate nurse involved subsequently quits nursing altogether…
Central line related air emboli have caused numerous preventable deaths. Awareness about this issue is limited, and solutions so far implemented have had limited effect. There is a need to appreciate the complexity of our work environments and apply human factors engineering to prevent these iatrogenic avoidable complications.
There were 14 reported incidents with 6 preventable patient deaths between January 2012 and April 2015 in NSW public health facilities from actual or suspected air embolism related to central line management. (1)
When presented with this cluster of adverse events one might question:
1. How are they happening?
2. Why has this issue remained relatively undetected?
3. Are these events widespread?
4. What has been done to prevent these events?
5. What should be done to prevent these events?
1. How are they happening?
Two conditions must be present for an air embolism to occur:
1. Direct communication between the atmosphere and the circulatory system; and
2. The presence of a pressure gradient that favours air entry into the circulation.
It is estimated that a volume of air as small as 70 mL in an adult can be fatal. The literature references a range of 70 to 500mL of air. A volume of 100mL of air per second may enter the circulation through a 14 gauge catheter with a pressure gradient of only 3.7mmHg (5 cm of H2O). Unfortunately the cardiac arrest that often results is frequently intractable.
Of the six deaths reported in NSW, four deaths were related to central line removal, one death was related to insertion and one during routine care processes. (1)
Removal:
Air emboli events on central line removal were often related to patients being in an upright position. Patients co-morbidities may make it difficult for them to tolerate the trendelenburg position or even lying flat.
Routine Care:
Several events occurred when lines were disconnected from their attachments and accidentally left open to air. Procurement of specific equipment could completely remove this risk.
Insertion:
Air emboli during insertion were more likely in spontaneously breathing patients having large bore catheters (e.g. Vas Caths) inserted. Positive pressure ventilation may reduce the risk in patients having these procedures under general anaesthesia.
Patient types:
Patients with respiratory pathology or intravascular depletion (generate greater negative intrathoracic pressures), and patients with a low body mass index (smaller venous tract between the atmosphere and vessel) feature prominently.
2. Why has this issue remained relatively undetected?
Air emboli may occur more frequently than we are aware. Cardiovascular collapse may often be attributed to other causes given the premorbid state of patients requiring central lines. For an air embolus to be suspected, staff need to be present at the time, who consider this as a differential diagnosis.
An echocardiogram demonstrating air in the cardiac chambers is often unlikely to be performed given the acute nature and location of most events.
If air embolism is suspected as a cause of death the pathologist should be notified so that the organs can be opened under water to detect escaping gas.
3. Are these events widespread?
In the international literature incidence rates for central line related air emboli range from 1 in 47 central line insertions to 1 in 3000 with some sources implying incidence rates as high as 0.1-2.0 per cent of all central lines used. (1)
A cluster of central line related air emboli have been reported in Pennsylvania, USA (2) and now NSW. It is likely that they occur at similar frequencies across all hospitals. As staff become more aware of the issue we may observe an initial increase in reported incidents.
4. What has been done to prevent these events?
Given that air embolism events continue to occur solutions in addition to those already implemented are required.
Root Cause Analysis:
Reported cases will often lead to a Root Cause Analysis (RCA). RCA is a time consuming process which, in NSW, has a mandated turnaround of 70 days. As a consequence, limited local patient safety resources spend a lot of time investigating incidents and then have to quickly generate recommendations. The RCA process is hindered by hindsight bias, risk of premature conclusion, failure to follow up, focus on the wrong contributing factors, and may lead to ineffective and non-sustainable solutions. (3)
Medical Alerts:
Several medical alerts have been disseminated in the past.(4,5) Medical alerts can provide education about adverse events and how they may be avoided. They may also prepare staff to be more understanding of subsequent procedural changes. On their own they tend to have limited effect in preventing adverse events. Medical alerts may fail to reach front line staff due to breaks in communication chains, and feedback mechanisms to assess for this are seldom in place.
Medical alerts have a temporal constraint, being viewed upon their initial dissemination, then become lost amongst other alerts and policies.
Protocols
Health care staff often work in complex environments, and at several different institutions. Each institution may have a similar protocol addressing the same issue. Many staff will be unaware of the existence of particular protocols or how to access them.
Protocols may not pay due respect to their workability. There may be a large ‘gap’ between ‘work as perceived’ by the protocol developers and ‘work as performed’ by front line staff. For example, protocols which, correctly indicate that patients should have their central line removed in the supine or slight trendelenburg position do not provide an option when this position cannot be tolerated. It is then left to the staff member to breach the protocol, often without realising the potential severe implications.
Perhaps prompting a procedural escalation when patients cannot lie supine or when their observations are outside pre-set variables would be prudent (e.g. contact senior medical staff, consider delaying removal, use increased levels of monitoring with ready access to resuscitative equipment).
Protocols, if used at all, need to be succinct, simple, workable, readily accessible, centralised, and recognisable across numerous healthcare facilities.
5. What should be done to prevent these events?
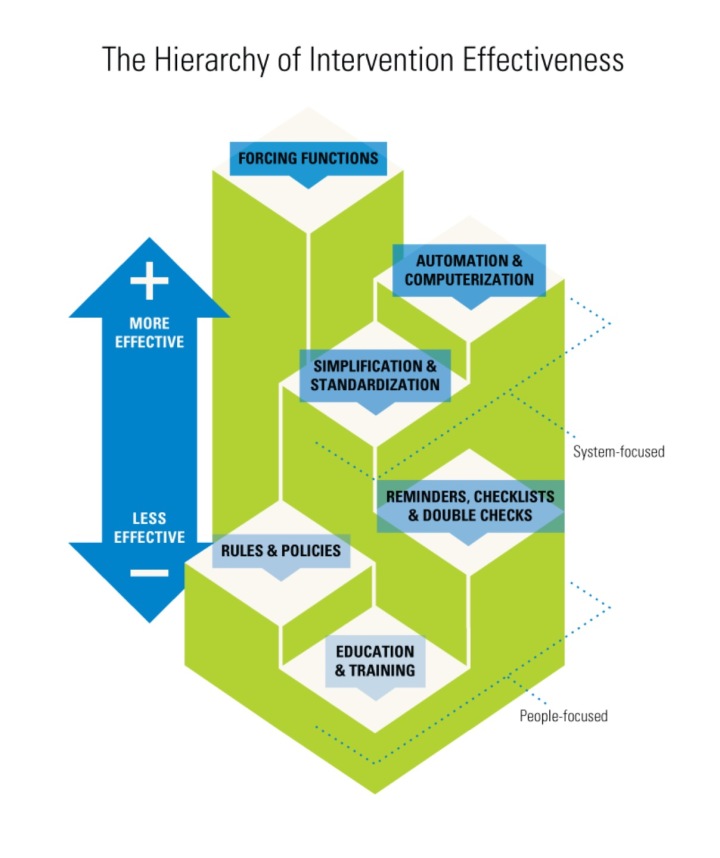
The complexity of our work environments needs to be appreciated and human factors engineering utilised in creating effective sustainable safety solutions. It is essential to understand that there is a hierarchy of intervention effectiveness from the most effective – system focused ‘forcing functions’ through to the least effective people focused ‘education, training and policies’. (Fig 1)
Procurement:
The risk of air embolus from accidental central line detachment during routine care can be eliminated by abolishing all central lines and attachments that have the ability to be left open to air and replace them with those that cannot. Unless vascular access devices are being used for pressure manometry they do not need to open to air. In human factors engineering this intervention is considered as a system focused ‘forcing function’ as it prevents the user from making the mistake – it is a highly effective safety intervention.
Central lines and attachments with moulded valves that can be swabbed also offer an advantage in decreasing Central Line Associated Blood Stream Infections.(Figs 2 & 3)
Centralised Central Line Management Form and Audit:
In 2011 the NSW Department of Health published an excellent policy directive entitled ‘Central Venous Access Device and Post Insertion Care’. (6) It outlines the salient features of central line management with respect to their risks. It also refers to the ‘Central Venous Line Insertion Record’ (7) – a valuable form for documentation. The use of this form should be encouraged throughout all hospitals in NSW.
Implementation of forms or e-health places time stress on staff. In that context the ‘Central Venous Line Insertion Record’ could be streamlined to focus on the important aspects of central line management from request through to removal, with documentation of the most useful data. A more powerful tool can be developed for reviewing the processes and equipment used.
Centralised Decision Tree:
Several decision trees exist (8) indicating if a central line is indicated and which vascular access device should be requested for a particular situation. The morbidity and mortality attributed to central lines appears underestimated, and consequently patients may die from central line complications when a central line is not required. Existing decision trees overlook ‘stepping down’ with the invasiveness of requested line – e.g. if a PICC line cannot be inserted serial peripheral cannulation may be more appropriate than a central line.
Ideally, there should be one centralised decision tree with which all staff are familiar across hospitals. It should be adaptable for use at particular institutions depending on the skills and facilities present.
Centralised Central Line Management Education and Accreditation:
The Clinical Excellence Commission, NSW Agency for Clinical Innovation, and Health Education Training Institute have developed a series of learning modules (see here) focussed on central line management. This centralisation of training and accreditation will be greatly beneficial to patient safety.
Effective Awareness Campaign
The majority of central line related air emboli reported in NSW occurred during line removal. Of these 9 cases, 7 of the patients were sat up whilst the central line was removed. In the remaining 2 cases the patient was sat up very quickly after removal.
An effective awareness campaign could be extremely useful in focussing staff on this point. Maybe ‘Central Lines Are Removed Supine‘, with an interactive animated screensaver, which succinctly explains how air emboli occur and the essential steps for prevention.(9) This could link to related educational material. Also perhaps a label, at the point of care, with the same message would be useful – we are looking for something that may be suitable so any suggestions most welcome.
In summary there is a great deal that can be done to improve safety with regards to central line management and decreasing patient exposure to the risk of air embolism. The implementation of effective and sustainable safety solutions requires an understanding of human factors engineering. We should focus on procurement of safer central lines and attachments and the importance of significant steps during central line removal particularly ensuring the patient is supine or slightly head down.




One thought on “Central Line Related Air Embolism – Applying Human Factors to the Design of Safe Systems”